In February 1950, the Journal of Ayurveda published an editorial severely chastising modern medical doctors. More than two years after independence, indigenous systems such as Ayurveda were beginning to receive partial state patronage. But it was becoming clear that the central and state governments in India had decided to continue with modern medicine as the official “state” medicine. The Journal appeared especially offended by a speech by Chamanlal Mehta, President of the Indian Medical Association (IMA).
While Ayurveda proponents were yet to reach a consensus about what to include in the curricula of Ayurvedic medical colleges, Mehta argued that building such colleges meant that “large amounts of money are being wasted.” In response, the editors of the Journal wrote: “Our advice to Dr. Chaman Lal is to leave our country and to proceed to England with the foreign pathy which he so dearly hugs to his bosom.” [1]
In the 1940s and the early years of independence, the majority of people in India primarily depended upon local and traditional therapies for many ailments, and often took recourse to modern medicine as a last resort. Even now, when modern medicine dominates public health and medical care provision in India, the demand for indigenous medical therapies, or products sold in the name of indigenous medicine, remains strong, as the public response to Covid-19 has shown.
So, if we sift through the hyper-nationalist discourse of the Journal of Ayurveda, the editors’ beef reveals an intriguing historical question: How did India end up choosing modern medicine in 1947?
If you are on daily blood pressure medications, or regular insulin therapy, or have been to a dialysis centre recently, this might feel like a moot question, with the answer self-evident in the efficacy and generally rational nature of modern medicine. But, for India in the 1940s, modern medicine was not as obvious a choice as it seems. Remember that, when the Journal of Ayurveda was arguing with Chamanlal Mehta, this system was relatively novel, inextricably associated with the coloniser, and faced healthy competition from modernising indigenous traditions.
Let me tell you the story of the remarkable trajectory of modern medicine (or biomedicine) in colonial India, ending in its political triumph at independence. Modern medicine became our primary system of medicine not because of some inevitable falling in place of things, but because of purposeful choices of people and communities. These active adopters and adapters of biomedicine are the main protagonists of my essay: Indian doctors, the Indian public, and the Indian National Congress.
Doctors
round 1888, the family of a young man in western India was discussing what career he should take up now that he had matriculated. An elderly friend opined that the prestigious post of Diwan, which the man’s late father used to hold, could become his if he studied law and became a barrister. Studying in India would be a prolonged affair, so the friend suggested going to England. The young man was excited at the idea of sailing to England but was afraid that the law examinations would be difficult to pass. Could he not instead be sent to qualify for the medical profession, he asked gingerly.
His older brother shot the idea down: “Father never liked it,” he said. “He had you in mind when he said that we Vaishnavas should have nothing to do with dissection of dead bodies.”
Though this young man, Mohandas Gandhi, did become a lawyer, a number of other privileged Indians during this time were electing to study modern medicine. The first major modern medical training institutions in British India were established in the 1830s in Calcutta and Madras. Right from the beginning, it was clear that medical colleges and schools [2] were popular with young people in Indian cities. Who were these Indians and what motivated them to study medicine at novel British-Indian institutions, under British teachers?
In the nineteenth century, these were mostly young people from urban wealthy, dominant-caste communities. Medical colleges and schools were exclusively urban-based, and by 1900, there were four government medical colleges (in Calcutta, Bombay, Lahore, and Madras) and 11 government medical schools, along with some private institutions. [3] But since around 90 percent of India lived in rural areas, where few people had the resources to send a young adult to live and study in a city for years, modern medical education remained out of their reach by default.
Even in the cities, not all young men found it easy to study medicine. Student admissions in the early decades were dictated by what British officials considered—and what their Indian interlocutors told them—to be “respectable” castes and communities. Sifarish, or recommendations, also played an important role. In other words, one could study medicine only if one had the right social and economic connections. Unsurprisingly, almost all doctors in India in the nineteenth and early twentieth centuries were individuals from dominant castes and communities. In 1895, for example, 35 out of 63 Bombay doctors were Parsi. [4] In the 1880s, elite Indian women also began to enter the medical profession, primarily following the assumption that women patients would go to modern medical centres only if those had women practitioners. [5]
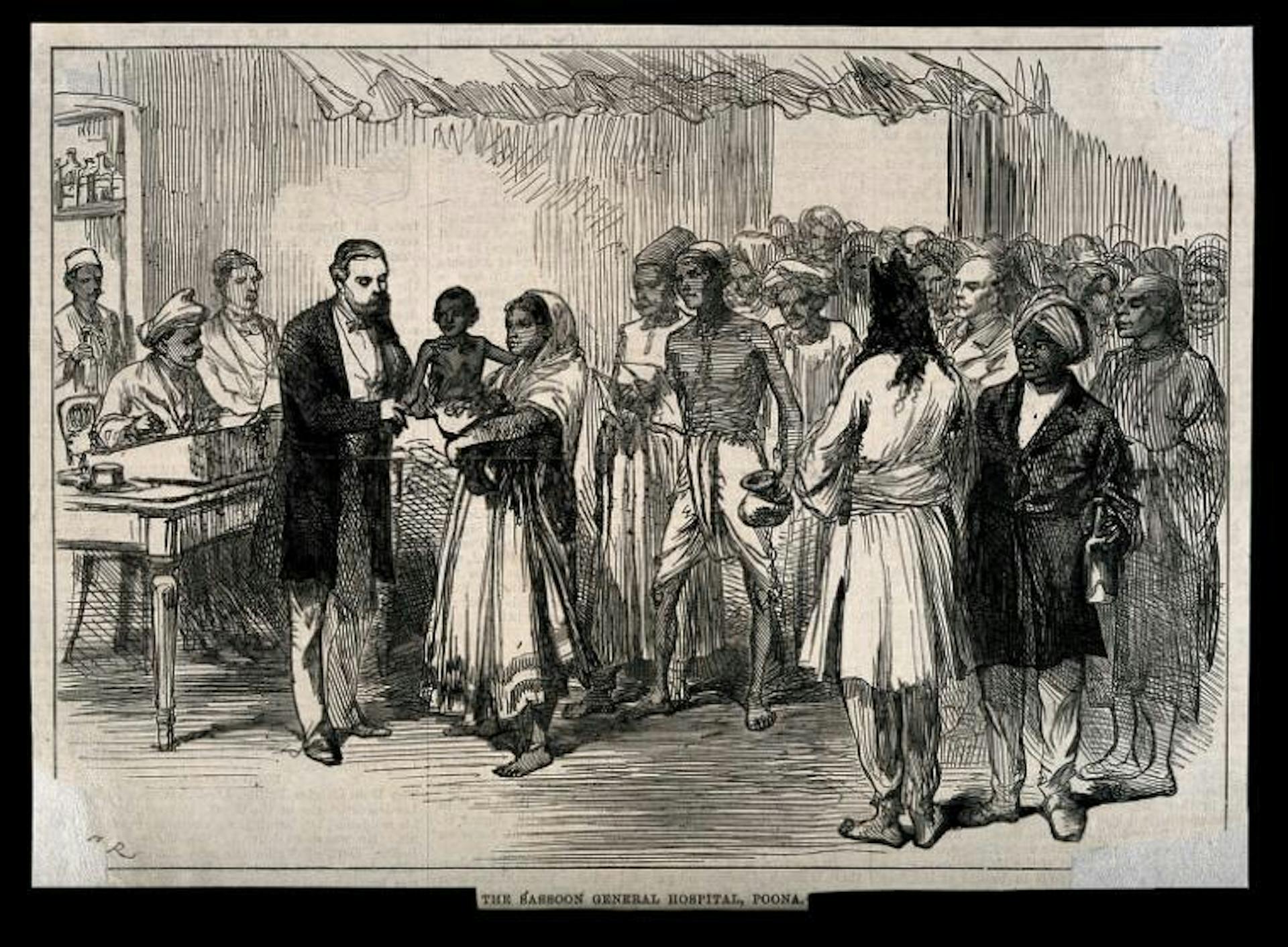
A wood engraving of patients awaiting treatment at the Sassoon General Hospital, Poona. It was published in an August 1879 edition of The Illustrated London News. Courtesy: Wellcome Library
As the Indian medical profession developed through the 1800s and early 1900s, it acquired a distinctly elite character in terms of class and caste, something which was already a general characteristic of indigenous hakims and vaidyas. [6] In other words, as has repeatedly happened in India, traditional caste privileges carried over even in an ostensibly modern version of a phenomenon.
A people who were considered literally untouchable outside the hospital were abruptly, transiently turned touchable, auscultable, operable, and dissectible.
The social composition of Indian doctors should explain why they chose modern medicine as an occupation in the first place. Modernity was a powerful force in India during the colonial period. The pursuit of status and power linked to modernity made well-off Indians pursue English-language education, study at British-Indian universities, make careers in colonially introduced professions, and participate in the colonial bureaucracy. These manoeuvres helped them maintain their historical socioeconomic privilege, even as the slightly more egalitarian structure of British administration was helping some oppressed castes begin to attain modest forms of economic mobility. [7]
In the case of modern medicine, it was initially the prospect of employment in the medical wing of the colonial military and in government hospitals and dispensaries that attracted many young Indians. Since medical learning in South Asia was traditionally restricted to certain families and confined to particular region-specific castes and communities, modern medical colleges and schools offered a way for individuals of other (mostly still privileged) castes to take up medical practice as a vocation. Doctors also soon realised that private practice in cities and towns could be convenient and lucrative, sometimes more so than government service. In the absence of a specific legal framework around medical licensing and registration, even medical students who had dropped out or failed the final exams did well as private practitioners in the mid to late 1800s.
Among those who graduated and chose private practice was Bombay’s Bhau Daji Lad, after whom Mumbai’s oldest museum is named. A Lancet article from 1855 describes how he “had scarcely been appointed”––to a government post––“when he resigned, finding that his own industry and abilities were quite sufficient to command practice, without the help of adventitious aid.” By the early 1900s, there were so many private doctors in major urban centres that some provinces began to disallow wealthier patients from accessing treatment for free in public hospitals, so that private doctors would receive a fair number of clients.
The autobiography of Muthulakshmi Reddy, a doctor and legislator in Madras, provides examples of successful Indian private practitioners. She writes, for instance, of M.C. Nanjunda Rao, who was a “popular practitioner in Madras and was earning thousands by his private practice.” As a young medical student, Reddy would often visit Rao’s “palatial building at Mylapore.” Rao lived in “very royal style owning 16 horse-carriages and an electrical plant for lighting his building.” The doctor had many “dependents,” and Reddy claimed there would be 60 people to feed daily at the house, even as Rao entertained dozens of guests. His wife would cook for them as she waited “for her husband’s arrival late in the afternoon from his wide practice.”
The financial success of Dr. Rao and others was aspirational—it made many young medical students consider private practice as a career of choice. By 1946, more than 70 percent of all Indian doctors were estimated to be in private practice. [8]
This was how elite, mostly dominant-caste Indians helped the British launch the trajectory of modern medicine in India. They championed it primarily in pursuit of the social status, power, and financial stability that medical practice offered. By the early 1900s, they had fashioned a socially and culturally powerful indigenous profession for themselves. With the establishment of the Indian Medical Association in 1928 and the All-India Medical Council (later the Medical Council of India, or MCI) in 1933, this profession could begin speaking in a collective voice.
Patients
ometime in January 1924, an inmate of a prison in Poona was seriously ill with fever and abdominal discomfort. The jail doctor exhausted all his options and reached out to the Civil Surgeon, Col. Maddock. The call, consultation, and the subsequent tests took a day or two, by which time the patient seemed to have gotten slightly better. But the next day he deteriorated, and the surgeon suspected the life-threatening possibility of acute appendicitis. An emergency operation was necessary. It was conducted by Maddock and two assistant surgeons, one of them Indian, in the Sassoon Hospital on a Saturday at around 10 in the night, and revealed a “suppurating” appendix.
Life-saving surgery had become increasingly common in Indian cities as the twentieth century dawned. But we know far more details of this particular patient’s experience than of innumerable others because he was Mohandas Gandhi, the man who’d once considered a doctor’s life for himself. By this time, of course, he had studied law in England, practised in South Africa, and returned to India a vastly different person from the 19-year-old who’d wanted to study medicine. [9]
Most histories suppress or ignore the voices and stories of some or the other major actor. In medical history, it is patients’ stories that are most frequently missing. For a long time, the discipline was dominated by medical doctors dabbling in history. In recent decades, however, that imbalance has been somewhat redressed by the interest and efforts of professional historians. As a result, we now have reasonable knowledge about how modern medicine was received and perceived by people in colonial India, even as more work by inventive scholars continues to enlighten us.
When the colonial government established the Madras school and Calcutta college in the early 1800s, its primary objective was to train Indian students to serve as subordinates of European doctors for the East India Company’s military needs. But it soon became clear that the “natives” were not averse to trying out modern medicine for their ailments. Bhau Daji’s hugely successful private practice would not have been possible if ordinary Indians in Bombay had refused to give his modern methods a trial. Besides, many Indian practitioners combined their modern medical knowledge with traditional Indian medical ideas, which further contributed to their warm public reception.
People in cities and towns generally encountered modern medical practice through public hospitals and private doctors. In rural areas, there were dispensaries and, in many cases, Christian missionary clinics. But the immense diversity of the Indian subcontinent meant that reactions to modern medicine differed widely.
A letter to the editor of The Times of India by Bombay-based doctor Bhalchandra Krishna, written in 1888, highlights the range of Indian response to modern hospitals. Among the many factors “injurious to the popularity” of hospitals, he listed the “intermingling of different castes in the same wards, and the consequent dread of losing caste” as an important one.
Other factors included the ministering and “close touch” of ward boys and servants who usually were from the “lower” castes; the “dread of death” induced by the fact that patients with ordinary ailments were often adjacent to serious patients in the wards; and the “dread of surgical, particularly of major, operations, and more especially of amputations and post mortem examinations.” Finally, he wrote, “high-caste” persons also found repulsive the “inferior” quality of diet and clothing provided for hospital patients. [10]
Remarkably, during and even after the colonial period, the majority of patients who utilised urban public hospitals, in the process offering “teaching material” to medical students and doctors, were from underprivileged castes and communities. The imposing edifice of the Indian biomedical profession was built, thus, almost entirely upon the backs and bodies of Indians from oppressed castes. A people who were considered literally untouchable outside the hospital were abruptly, transiently turned touchable, auscultable, operable, and dissectible by the very elites who had relegated them to a manufactured [11] backwardness.
Despite variations in reception, and a substantial number of Indians having never encountered modern medical therapies (including hundreds of Adivasi communities who depended on their own knowledge and skills for medical matters), modern medicine had acquired broad public acceptance in India by the early 1900s. The administrative reports of hospitals and dispensaries showed upward trends in patient numbers year after year, and scores of wealthy Indians chose to fund new dispensaries and hospitals as part of their charitable activities.
It was during this time that popular individual doctors, such as Nanjunda Rao in Madras and Bidhan Chandra Roy in Calcutta, began to “command a roaring practice.” [12] Famous clinics like Shroff’s Eye Centre (Delhi) were also established in this period. In Bombay, the Bai Jerbai Wadia and the Bai Yamunabai Laxman Nair hospitals were founded. Private nursing homes and clinics were also on the rise around the country, indicating a thriving middle- and upper-class marketplace for the services of doctors.
The early part of the twentieth century was in fact a tremendously successful period for modern medicine around the world. Surgical procedures were becoming increasingly safe and effective with improvements in anesthesia and asepsis [13] and new chemotherapeutic drugs were transforming excruciating ailments into tolerable conditions. In parts of India, for example, the debilitating and widespread disease of kala azar, or visceral leishmaniasis, began to be managed with injectable drug regimens, including one introduced by physician Upendranath Brahmachari, an alumnus of the Calcutta Medical College. Many Indians experienced injections for the first time, and the practice came to be associated with quick relief and effectiveness. [14]
This broad hegemony of modern medicine was reinforced by popular movies produced in Calcutta and Bombay. In Dr. Madhurika (1935), the eponymous doctor was a “modern” Indian woman, surgeon, and birth control advocate. It was perhaps the first Indian movie to feature a doctor as protagonist. [15] In 1936, Achhut Kanya showed a village shopkeeper selling quinine—which was then a “wonder drug”—to sick villagers, confidently telling them that there was no better cure for malaria.
Dushman (1939) featured Prithviraj Kapoor as a maverick doctor who successfully treats tuberculosis patients with unconventional methods. The Pankaj Mullick saga Doctor (1941) was centred around the relationship between a father and son, both physicians. The superstar Ashok Kumar also played a doctor in two films in the early 1940s (Anjaan and Najma). In all of these movies, modern medicine was overwhelmingly portrayed in a positive light, as a crucial science indispensable to India’s progress.
The popularity of modern medicine did not mean, however, that it completely replaced indigenous medical therapies. Hakims and vaidyas remained important care providers for many people. So did bone-setters, dais, ojhas, bhagats, shamans, babas, and others––the wide variety of practitioners reflected the vibrant history of how different communities and geographies had evolved different ways of caring for their sick.
Compared to around 47,500 modern medical doctors at the turn of independence, there were around 2-2.5 lakh practitioners of Ayurveda and Unani, in addition to homeopathy practitioners, Adivasi healers, dais, bone-setters, etc.
Homeopathic practitioners had also grown popular in some regions of the country. Clearly, the people of South Asia had simply added modern medicine to their existing list of options. Their use of it was rarely dictated by some firm conviction that it was the “best” form of care. Such “medical pluralism” remains a defining feature of how people think about medical care in most of the world. It exists because people use multiple forms of rationale when choosing which provider to visit: ease and availability, practical efficacy, religious and other sectarian beliefs and prejudices, and the interpersonal behaviour of practitioners.
It is highly likely that even in the early decades of the twentieth century, the number of people who visited modern medical doctors was less than those who accessed care from other providers. Compared to around 47,500 modern medical doctors at the turn of independence, there were around 2-2.5 lakh practitioners of Ayurveda and Unani, in addition to homeopathy practitioners, Adivasi healers, dais, bone-setters, etc. [16]
Modern medicine remained concentrated in select urban and district centres of the country, and local indigenous providers were far more accessible for most people. Public hospitals had increasingly come to be associated with overcrowding, insanitary conditions and indifferent staff. At the same time, many indigenous practitioners, especially Ayurvedic and Unani physicians in cities and big towns, had responded enterprisingly and assertively to modern medicine—their own forms of modernisation had spurred popular interest in their practice.
So, around the time when India was marching towards independence on the political front in the 1930s, biomedicine was not the only form of medical care staking a claim for pre-eminence. The people of India seemed generally to be comfortable with modern medicine, yes, but diverse forms of indigenous medical care were also an important part of their lives and communities. With the public not decidedly leaning towards a single system, the battle for primacy had fundamentally come down to a debate between the elites: the leaders of the modern medical, Ayurvedic, and Unani professions—the three most institutionalised medical systems at the time.
As it turned out, the job of refereeing fell upon the Indian National Congress.
The Congress
n October 1938, the Indian National Congress, fresh from its massive victories in the provincial elections of the previous year, organised a conference of the Ministers of Industries with Subhas Chandra Bose as Chairman. The ministers resolved that a “comprehensive scheme of national planning” was needed to carry out industrialisation, which in the dominant opinion was the best way out of poverty and unemployment.
This planning was entrusted to a committee which became known as the National Planning Committee (NPC), chaired by Jawaharlal Nehru. While the early days of the NPC’s proceedings were dominated by concerns around industrial planning, healthcare entered their discussions during the second session in June 1939, and a sub-committee on “national health” was appointed.
The sub-committee’s composition left no doubts about the INC’s position in the medicine debate: all of the members were trained in modern medicine, or other modern sciences. The chairperson, Sahib Singh Sokhey, was a prominent Indian Medical Service (IMS) officer. J.S. Nerurkar, the secretary, was a professor at Seth G.S. Medical College, Bombay. Other members included the doctors B.C. Roy, Rani Laxmibai Rajwade, S. Abdur Rahman, and N.M. Jaisoorya. The sub-committee wanted to “set India on the road of scientific development in the domain of medicine,” it declared, with “scientific” specifically meaning the modern sciences. [17]
Other vocal elites of this time, including some from the INC, batted for a “national” or Hindu medicine. This, of course, translated to a monolithic Ayurveda—a sanitised, politically developed concept unreflective of the diversity of practices, ideas and treatises which had developed dynamically over centuries in different parts of the subcontinent. [18]
The prevailing misconception that Ayurveda was a purely Hindu and Vedic system of knowledge owed much to the flawed narratives of eighteenth and nineteenth century British Orientalists, and the efforts of nineteenth and twentieth century Ayurvedic practitioners to carve out a niche for themselves in the shadow of modern science.
But such claims were becoming increasingly common in the early 1900s, along with the ahistorical assertion that Ayurveda went into “decline” because of post-Ashoka Buddhist and later Islamic administrations. The elephant in the room was the caste system—beliefs around “unclean” persons, objects and activities, which included such stuff as touching bodily secretions and assisting in childbirth, were conveniently ignored. [19]
This increasingly shrill framing of Ayurveda in the early twentieth century as a narrow, religiously-defined medical ideology dampened the enthusiastic support of some INC leaders. Even Mohandas Gandhi, whose general pessimism about what he termed “European medicine” was well-known, was often critical. “Our hakims and vaids... follow without question formulas,” he said in a 1921 speech at the opening of an Ayurvedic and Unani college in Delhi. “They carry on little [scientific] investigation. The condition of indigenous medicine is truly deplorable.” [20]
At the same time, many Unani physicians were claiming their system to be the most appropriate “national” medicine for India. [21] These “national” claims were being opposed by prominent regional practitioners, like those of the Tamil Siddha and the Punjabi Baidak. [22]
The widespread belief in the stagnancy of indigenous medical systems—“pure” and unchanging for centuries—animated the writings and speeches of the proponents of modern medicine in the early 1900s. In recent years, this idea of timelessness has been challenged by historians who have shown that the indigenous traditions were neither stagnant nor based only on a few exalted classic texts. For example, there was a substantial exchange of ideas and drugs between Unani and Ayurvedic practitioners during the Mughal period. Unsurprisingly, ordinary medical practitioners were generally enterprising. They looked for new ways to practise their healing arts and craft.
This more nuanced understanding, however, was not common in the early twentieth century, and the supposed stagnancy of indigenous medical practices became one of the decisive points in the larger debate on the primacy of medical systems. NPC health sub-committee member S. Abdur Rahman, while praising the past utility of the Ayurvedic and Unani systems, wrote that the practitioners of these systems, except a few “pioneers,” had failed to assume a “scientific outlook.” In the considered opinion of the NPC modernists, free India’s “national” medicine had to be the “international” modern scientific system of medicine.
The Bhore Committee’s final four-volume report, released in early 1946, has since become the stuff of legend in Indian medical and public health circles.
Not long after the NPC sub-committees had drafted their provisional reports in 1940, the Quit India movement got underway and major Congress leaders were imprisoned. By the time they were released in the middle of 1945, the situation in India had radically changed, not just politically, but also in terms of healthcare planning. In October 1943, the British Indian government had constituted a high-profile committee called the Health Survey and Development Committee, likely at the behest of Sardar Jogendra Singh, the member of the Viceroy’s Executive Council who was in-charge of the Education, Health and Lands department. The committee was chaired by the retired Indian Civil Service officer, Sir Joseph Bhore.
Although the Bhore Committee was part of the British colonial apparatus, only six of its 24 members were non-Indian. Bhore himself was a seasoned Indian bureaucrat whose early education had been at the Bishop’s High School and Deccan College in Poona. In terms of technical expertise, the committee consisted only of members trained in modern medicine. Its final four-volume report, released in early 1946, has since become the stuff of legend in Indian medical and public health circles. It forms an important part of the MBBS curriculum today.
While championing modern medicine as the official system of medicine for soon-to-be-independent India, the report said:
“We feel that we need no justification in confining our proposals to the country‐wide extension of a system of medicine which, in our view, must be regarded neither as Eastern nor Western but as a corpus of scientific knowledge and practice belonging to the whole world and to which every country has made its contribution. We feel that it would be unfair and unjust… to deny to anyone in this country the benefit of the scientific system and of the daily growing volume of research and achievement in the wide world of science.”
Looking back, the Bhore report was a next to last push. One thing remained before India’s adoption of modern medicine was made properly official: popular political support. Despite its overwhelmingly Indian composition, the Bhore Committee was an arm of the departing British Indian government. For its report to have credence in independent India, it needed to be ratified by elected Indian representatives.
That opportunity arrived in October 1946, at a three-day conference of provincial Health Ministers. [23] Not only was the Bhore report unanimously approved, the committee’s recommendations for future health policymakers were also endorsed. Indigenous medical systems got only a brief mention at the conference, with the ministers recommending that the government establish educational institutes for these systems and fund further research “on scientific lines.”
The modernist in Nehru would have been pleased with these developments. “The indigenous systems may have excellent remedies for certain ailments, but they lack scientific basis,” he told the Association of Physicians of India in February 1947. “People talk of allopathy, homoeopathy and various other pathies and methods. But what is important is—are you going to follow a scientific method or not?”
There were other compelling reasons for Indian politicians and administrators to place heavy reliance on modern medicine. For one, it would have been a political nightmare to reconcile the competing demands for primacy of not just Ayurvedic and Unani practitioners, but also of the several other indigenous practitioners and systems that existed in the vast Indian medical space. From an administrative point of view, it would have been foolhardy to let go of the well-established colonial machinery in medicine and public health, including the medico-legal apparatus (consisting of post-mortem and associated forensic medicine infrastructure) that had penetrated every region of India.
Additionally, leaders could not imagine improving the country’s crucial health indices like maternal and infant mortality, managing and preventing deadly infectious diseases, and encouraging an industrial workforce with its attendant accidents and injuries, without the aid of modern medical interventions.
Introduced as a colonial necessity, modern medicine was quickly adopted and propagated by elite Indians, gradually (sometimes grudgingly) adapted and utilised by the Indian public, and eventually, in 1946, “officiated” as free India’s primary method of healthcare by the country’s political leaders.
ike other decisions taken in the heady months of the late 1940s, this one has been fiercely debated over the decades, especially in terms of the “stepmotherly” treatment meted out to Ayurveda by successive governments. [24] Much of the anti-biomedicine critique in the last few years, however, uplifts primarily Ayurveda and ignores other forms of indigenous medical traditions, including the medical practices of Adivasi communities. Besides, Ayurvedic practice has proven equally susceptible to issues that plague biomedical practice, including profiteering and patient exploitation.
It is probably not an exaggeration to say that without the Indian state’s heavy investment in modern medicine and public health, a great number of people from our parents’ and grandparents’ generations would not have existed. The population of India in 1947 was some 36 crore and life expectancy was around 32 years. Today, with a population of around 136 crore, India’s life expectancy is almost 70 years.
Yet, the horrible precarity of life which marked the early years of independence is not exactly history. Underprivileged people continue to suffer from severe complications of curable or manageable illnesses, and die easily preventable deaths. [25] This is unnecessary suffering, caused largely because there is no political will to make curative and preventive measures affordable and accessible. The experience of privileged India over the last 70 years [26] shows that modern medicine, coupled with basic public health measures like clean water and nutritious food, possesses a transformative capacity to reduce preventable deaths and make people’s lives less infirm in general.
The devastating second wave of Covid infections in India has validated the life-saving nature of biomedical treatment, and vindicated the wisdom of those who decided to adopt it as state medicine in the 1940s. Yet, over the last few weeks, we have seen how affordability and accessibility issues plague biomedical therapies. Politics, policymaking and class and caste networks overwhelmingly influence which lives are saved by biomedicine, and which are ignored.
The sheer life-saving nature of modern medicine makes it a tremendously important public good. Our founders recognised this and embarked upon the task to make modern medical care equitable, accessible, and affordable for all. The Bhore report proposed “a comprehensive health service offering preventive and curative medical care to all, irrespective of their ability to pay.” Rajkumari Amrit Kaur, India’s first health minister, was a tireless champion of modern medical institutions. In her time, she laid the foundations of some of our most dependable public health infrastructure.
Now, 65 years on, as institutional deficiencies lie exposed by the pandemic, it sinks in that later generations of leaders have come nowhere close to delivering the promises of our founders. India’s collective misery today has made it clear that, in the coming years, the completion of that crucial task—universal healthcare—needs to be the foremost priority for both its public as well as its policymakers.
Kiran Kumbhar is a physician and writer currently in a PhD programme, studying the history of medicine and science.